Peritoneal Dialysis
Treatment Overview
Peritoneal dialysis uses a membrane inside your body (peritoneal membrane) as a filter to clear wastes and extra fluid from your body and to return electrolyte levels to normal. Unlike in-center hemodialysis, you do not need to travel to a dialysis center for your treatment. Instead, after being trained at a dialysis center, you will do your treatment at home on your own schedule. Peritoneal dialysis can often be done at night, while you are sleeping.
You will need to have a catheter placed in your belly (dialysis access) before you begin dialysis. Placement is usually done 10 to 14 days before dialysis starts. Some peritoneal dialysis catheters may be used immediately (acute-use catheters). But because of a high risk of complications, these catheters are not commonly used.
The process of doing peritoneal dialysis is called an exchange. You will usually complete 4 to 6 exchanges each day using the following steps:
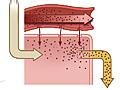
- Fill: Dialysis fluid enters your peritoneal cavity.
- Dwell: While the fluid is in your peritoneal cavity, extra fluid and waste travel across the peritoneal membrane into the dialysis fluid.
- Drain: After a few hours, the dialysis fluid is drained and replaced with new fluid.
There are different types of peritoneal dialysis. Discuss these treatment methods with your doctor to decide which one might work best for you.
- Continuous ambulatory peritoneal dialysis (CAPD). During CAPD, the dialysate solution stays in your belly for about 4 to 6 hours. After this time, the solution is drained out of your belly. Your belly is then refilled with fresh solution. You need to change the solution about 4 times a day. This is the most commonly used form of peritoneal dialysis.
- Continuous cycling peritoneal dialysis (CCPD). During CCPD, a machine automatically fills and drains the dialysate from your belly. This process takes about 10 to 12 hours, so you can do CCPD at night while you sleep.
Choosing between treatment with hemodialysis or peritoneal dialysis is based on your lifestyle, other medical conditions, and body size and shape. Talk to your doctor about which type would be best for you.
Why It Is Done
Peritoneal dialysis replaces the work of the kidneys after complications of kidney failure develop.
How Well It Works
Peritoneal dialysis provides approximately 10% of normal kidney function. It does not reverse chronic kidney disease or kidney failure.
Risks
The most common complications from peritoneal dialysis include infection around the catheter site or infection of the lining of the abdominal wall (peritonitis). Less commonly, there may be problems related to the catheter. But most complications can be managed or prevented.
Peritoneal dialysis is not recommended when any of the following conditions are present:
- Scarring of the lining of the abdominal wall (peritoneal membrane)
- Leaks in the lining of the abdominal wall
- Active inflammatory bowel disease (Crohn's disease, ulcerative colitis)
What To Think About
Peritoneal dialysis is a good treatment option for people who have kidney failure. Advantages include:
- Few dietary or fluid restrictions.
- No needle sticks.
- Independence and ability to normalize daily routines.
- The ability to do the dialysis at home.
- Reduced dependence on blood pressure medicine.
- Fewer problems with anemia.
Current as of: March 15, 2018